BioSocial Health J. 1(4):204-211.
doi: 10.34172/bshj.34
Original Article
A randomized controlled study on the effectiveness of a diabetes self-management app in Bangladesh
Bilkis Banu Conceptualization, Data curation, Formal analysis, Methodology, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, 1, * 
Nasrin Akter Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Validation, Visualization, Writing – original draft, Writing – review & editing, 2
Sujana Haque Chowdhury Conceptualization, Data curation, Formal analysis, Investigation, Project administration, Visualization, Writing – original draft, 2
Nusrat Hossain Sheba Data curation, Investigation, Project administration, Visualization, Writing – original draft, 2
Md. Abdul Hakim Majumder Funding acquisition, Resources, Supervision, Writing – review & editing, 2
Author information:
1Department of Public Health, State University of Bangladesh, 696 Kendua, Kanchan, Rupganj, Narayanganj, Dhaka-1461, Bangladesh
2Department of Public Health, Northern University Bangladesh, 111/2 Kawla Jamea Mosjid Road, Dakshin Khan, Uttara, Dhaka, Bangladesh
Abstract
Introduction:
The smart phone application concept is widely recognized as a tool to support patients’ adherence. Using different types of reminder-based materials combined with traditional health education has demonstrated its effectiveness in enhancing knowledge and fostering adherence to diabetes management. Very few studies found to identify the effectiveness of smartphone application for the diabetes seven self-management components. This study was aimed to assess this issue among Bangladeshi patients.
Methods:
A randomized controlled trial was performed from July 2022 to June 2023 in two diabetic hospitals affiliated with the Diabetic Association of Bangladesh located in Dhaka district among the 400 diabetic patients. The smartphone Application ‘Diabetes Self-Care’ was installed on the smartphone of each patient of the intervention group and instructed them to use it. Data were collected using a semi-structured questionnaire through face-to-face interview. Knowledge and adherence were measured and compared in the different groups before and after the intervention using t-test, McNemar’s test, and logistic regression technique.
Results:
The endline status of the intervention group reflected significant (P<0.01) improvement in knowledge and adherence to self-management compared to the baseline status. Knowledge (regarding seven self-management components, basic and technical components of diabetes) improved significantly (P<0.01) in the intervention group. Adherence to self-management components improved significantly (P<0.01) more in the intervention group than in the control group.
Conclusion:
The m-Health intervention, using smartphone application, demonstrated a noteworthy enhancement and positive impact on patients’ knowledge and adherence. This successful model of intervention holds the potential for nationwide replication, offering a viable approach for self-managing diabetes and other non-communicable diseases to enhance patient outcomes and reduce healthcare burdens.
Keywords: Smartphone application, Self-management, Diabetes mellitus, Randomized controlled trial, Bangladesh context
Copyright and License Information
© 2024 The Authors.
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
The study was funded by the Ministry of Science and Technology, Peoples’ Republic of Bangladesh.
Introduction
Diabetes mellitus (DM) is one of the most common and prevalent chronic diseases in the world.1,2 With 7.1 million diabetic individuals, Bangladesh is the country with the 10th-highest prevalence of adult diabetes worldwide. Its prevalence in Bangladesh is also increasing (5.52% in 20133 and 7.4% in 20154) and rising costs for complications (41 USD in 20133 and 51 USD in 20154) can be avoided with early diagnosis and adequate management. Diabetes has no cure, thus self-management is essential throughout one’s lifetime.2,5 Self-management covers things like foot care, food, medication, physical activity, follow-up appointments, blood glucose tests, and avoiding risky behaviors. By doing these things, one can lessen problems, enhance glycemic control, and enhance one’s quality of life. To change patients’ behaviors and increase their engagement in their treatment, diabetes self-management education and support are crucial, especially at the time of diagnosis.5,6 The Diabetic Association of Bangladesh (BADAS) has already begun implementing many diabetes control projects in Bangladesh, although no outcomes have yet been made public.7 Mobile phone use could be a low-cost way to give patients more control over their diabetes care.8-11 Mobile health (m-Health) or electronic health (e-Health) initiatives using mobile phones to improve health have recently spread the world.12 Bangladesh, which has 159 million people overall but 150 million mobile phone subscribers, may readily adopt this technology as an option.8,9 The m-Health approach appears to work well in cities and among educated young individuals13,14 including rural regions.15 A study in a developed country demonstrated that using the mobile app “bant II” for self-management of type 2 diabetes mellitus (T2DM) helps patients monitor changes in their glycemic control, receive guidance on corrective actions, and improve their overall self-management skills.16 Moreover, a study conducted in Iran found that T2DM patients in developing nations had a positive outlook and high level of confidence when using health management apps on smartphones will help them control their diabetes.17 In addition, a study among Australian patients indicated that despite various hurdles such as technical difficulties including initial setup, and poor internet access, the majority of app users had improved self-management and health after using the program.18 Several review articles suggest that mobile app-assisted self-care interventions are effective for managing blood glucose and blood pressure by facilitating remote health management, communication, personalized recommendations, and decision-making.19 Diabetes education material in the form of self-management apps is rapidly evolving, and integrating into healthcare service delivery where digital technologies and self-management solutions have become increasingly important.20 Numerous smartphone apps based on self-management strategies for DM have been developed globally but not concerning the seven self-management components. In Bangladesh, a middle-income country, there are many various cultures and religions, as well as vast differences in socioeconomic status and access to medical care depending on where you live. At the same time, the number of diabetics in Bangladesh is rising. There are no studies that show how well smartphone applications help to control their diabetes The improvement in the diabetes patient’s knowledge and behavior, together with the behavioral change method, will demonstrate the effectiveness of the smartphone application “Diabetes-Self Care.” This present study intended to explore the effectiveness of this smartphone application (including seven diabetes self-management components) in managing patients’ daily in diabetic condition and thereby empowering diabetic population in Bangladesh.
Methods
Study design
This study employed a randomized controlled trial based on communication technology, encompassing both an intervention and a control group. The study was conducted in the Dhaka district, the capital of Bangladesh. The district boasts urban and rural distributions, supported by ample technical and logistical resources followed by the administrative layer.21
Adhering to the Declaration of Helsinki, the study obtained approval from the Ethical Review Committee.
Participants
The study spanned a duration of 12 months, from July 2022 to June 2023 with a baseline survey, an 8-month intervention phase, and an endline survey supervised by the Department of Public Health, NUB. The study included diabetic patients (both type 1 and type 2) registered at Savar Swasthoseba Kendro (SSK) and Bangladesh Institute of Health Sciences (BIHS) General Hospital, managed by the BADAS. Participants met specific inclusion criteria followed written informed consent: (i) diagnosed as diabetic according to the WHO guidelines (threshold values for fasting ≥ 7.0 mmol/L and for 2 hours fasting plasma glucose ≥ 11.1 mmol/L); (ii) registered in the SSK and BIHS General Hospital; (iii) residing in the Dhaka city and within 2 km of the study places; (iv) aged 18 to 64 years and (v) owning a smartphone with willingness to participate. Exclusion criteria encompassed: presense of gestational DM and mental or physical disability.
Randomization
A total of 400 participants, distributed 200 individuals in each group, was enlisted for the study. The sample size was determined utilizing the formula “n = ‘[2 X (a + b)2 X ℧2]/ (µ1-µ2)2” where a (conventional multiplier for alpha, 0.05) = 1.96, b (conventional multiplier power) = 0.842, ℧ (population variance) = 16.3 and (μ1− μ2) (population mean difference among two groups) = 4.57 detected with 80% power and 0.05 significance level.7
This study was conducted in Dhaka city to represent the diverse diabetic patient population. Initially, 400 patients were randomly selected from last year’s registered patient index (SSK = 973; BIHS General Hospital = 1610) of affiliated hospitals with BADAS. Patients were recruited in this study employing a systematic approach with intervals of five and eight between patients from SSK and BIHS General Hospital, respectively, meeting inclusion and exclusion criteria. If a patient didn’t meet the criteria, the next targeted patient was approached. After randomization, informed consent was obtained, and baseline data was collected. During the end line period, twelve participants were lost to follow-up: one died, and eleven refused to continue participation (Figure 1).
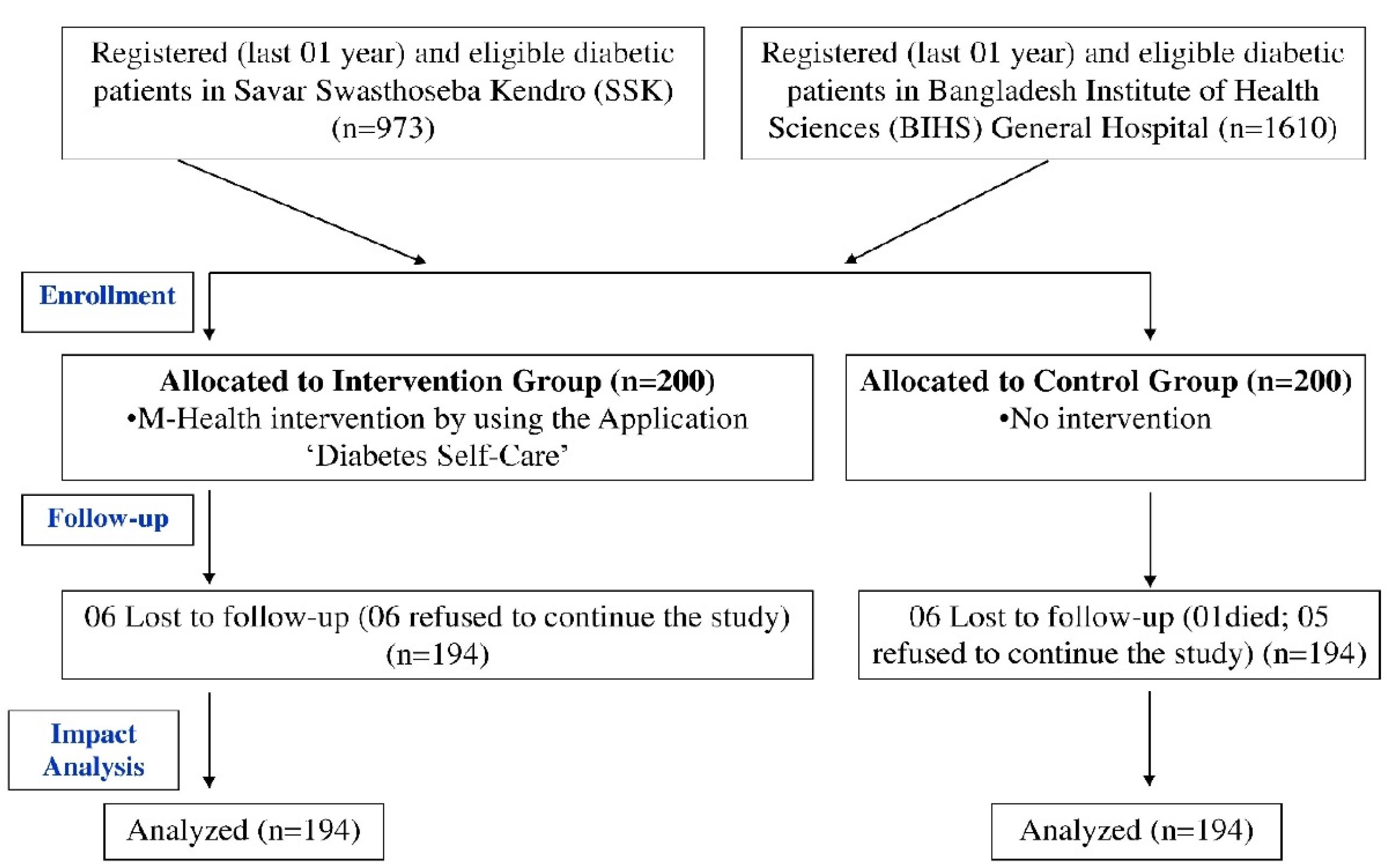
Figure 1.
Participant flow throughout the study
.
Participant flow throughout the study
Procedures
Baseline and end-line data were acquired through face-to-face interviews, employing a pre-tested and semi-structured questionnaire. Concerning the validation, the questionnaire was designed incorporating relevant variables adapted from previously published article and based on our research context.22 Data collectors obtained self-management practices, healthcare advice, and clinical measurements (blood pressure and blood glucose) from patients’ diabetic guidebooks. These guidebooks, standard for all affiliated hospitals under BADAS, contain updated physician advice and clinical information.
Each intervention group patient received the smartphone application “Diabetes Self-Care,” developed by the research team in collaboration with NUB’s Computer Science and Engineering department. The app, with distinct colors for each self-management component, reminded patients and guided their actions accordingly. Such as diet: timing and type; drug: dose, frequency, direction, and duration; physical exercise: name, timing, and duration; follow-up visits and blood glucose tests: date and interval; blood glucose monitoring at home: dates and times/days; tobacco avoidance: for not taking that a patient wanted to avoid; foot care: timing and type. Control group patients did not receive this intervention. A matrix sheet tracked patient progress, with three contact attempts within seven days. Reasons for missed contacts were documented. Patients could opt out at any time.
Outcomes
The outcomes of this study were: (i) basic and technical knowledge of diabetes, (ii) adherence to the advices of drug, diet, physical exercise, follow-up visit, blood glucose test, stop smoking and foot care. During the regression analysis, a model was adjusted, incorporating socio-demographic, disease and therapeutic, health services, and clinical characteristics of the participants.
Measures of this study
Knowledge: Knowledge assessment of diabetic patients involved a scoring system covering basic and technical knowledge. Basic knowledge included diabetes definition, types, blood glucose thresholds, symptoms, management, complications, and hyper- and hypoglycemia. Technical knowledge encompassed: drugs (dose, frequency, route, duration, expiry date), diet (frequency of meals, foods not recommended), regular physical exercise (frequency, duration, safety issues), benefits of attending follow-up visit and doing regular blood glucose test, importance and process of stopping tobacco consumption and advice for regular foot care. Each correct response scored 1, incorrect ones received 0, and for multiple correct answers, the score was divided by the total. The total score was converted into a percentage, categorized as poor ( < 50%) or good ( > 50%) knowledge.23
Adherence: Drug adherence included following prescription advice for dose, duration, frequency, and route (oral or injection). Dietary adherence meant having at least five meals per day, while physical activity adherence was at least ≥ 150 min/wk. Adherence also involved attending follow-up visits and blood glucose tests within seven days of recommendation, abstaining from tobacco use, and weekly foot care, which included checking feet and shoes and trimming toenails.22
Clinical information: The high blood pressure threshold was ≥ 120 mm Hg for systolic blood pressure (SBP) and ≥ 80 mm Hg for diastolic blood pressure (DBP).24 The blood glucose threshold two hours after breakfast was set at > 7 mmol/L.25
Statistical analysis
The data underwent rigorous quality checks, followed by entry and analysis employing the Statistical Package for the Social Sciences (SPSS). Continuous variables were presented as mean ± Standard Deviation (SD), while categorical variables as percentages with 95% confidence intervals (CI). Paired and independent t-tests compared means within and between groups, while McNemar’s test and logistic regression analyzed categorical variables. Statistical significance was set at P < 0.05.
Results
Participant’s characteristics
We included 400 participants (40.0% male and 60.0% female) in the study, where the majority (n = 230, 57.5%) had a family history of diabetes. No substantial or statistically significant differences were observed in the baseline characteristics of participants between the intervention and control groups, as indicated in Table 1.
Table 1.
Baseline characteristics of the study participants
|
|
Total (400)
|
Intervention group (200)
|
Control group (200)
|
P
value
|
|
Mean±SD or n (%)
|
Mean±SD or n (%)
|
Mean±SD or n (%)
|
| Gendera |
0.22 |
| Male |
160 |
40.0% |
86 |
43.0% |
74 |
37.0% |
| Female |
240 |
60.0% |
114 |
57.0% |
126 |
63.0% |
| Number of childrenb |
3 ± 2 |
3 ± 2 |
3 ± 2 |
0.42 |
| Family sizeb |
4 ± 2 |
4 ± 2 |
4 ± 2 |
0.06 |
| Family historya |
0.15 |
| Had |
230 |
57.5% |
122 |
61.0% |
108 |
54.0% |
| Didn’t have |
170 |
42.5% |
78 |
39.0% |
92 |
46.0% |
| Used therapya |
0.82 |
| Clinical (oral drug/ insulin) |
379 |
94.8% |
189 |
94.5% |
190 |
95.0% |
| Others (herbal/ homeopath) |
21 |
5.2% |
11 |
5.5% |
10 |
5.02% |
| Distance to go to hospitala |
0.64 |
| < 3 km |
302 |
75.5% |
149 |
74.5% |
153 |
76.5% |
| > 3 km |
98 |
24.5% |
51 |
25.5% |
47 |
23.5% |
| Cost to go to hospitala |
0.60 |
| < 0.74 USD |
249 |
62.2% |
127 |
63.5% |
122 |
61.0% |
| > 0.74 USD |
151 |
37.8% |
73 |
36.5% |
78 |
39.0% |
| Accompanying person neededa |
0.76 |
| Yes |
227 |
56.8% |
112 |
56.0% |
115 |
57.5% |
| No |
173 |
43.2% |
88 |
44.0% |
85 |
42.5% |
| Blood pressure (diastolic)b |
81.52 ± 14.02 |
81.22 ± 11.48 |
81.80 ± 16.20 |
0.25 |
| Blood glucose (fasting)b |
8.27 ± 2.90 |
8.21 ± 2.77 |
8.33 ± 3.03 |
0.92 |
a Data presented as proportion (n) and percentage (%); b data presented as mean ± SD; Statistical significance at P< 0.05; n for each group (intervention and control) = 200.
Respondents in this study mostly resided with family members and had an average of three children (family size: 4 ± 2, number of children: 3 ± 2). The majority (75.5%) found the hospital conveniently close ( < 3 km), but most (56.8%) stated they needed an accompanying person while visiting. Almost all participants (94.8%) were using clinical therapy, with the treatment cost ( < 0.74 USD) being affordable for the majority (62.2%). Additionally, clinical parameters such as blood pressure (diastolic: 81.52 ± 14.02) and fasting blood glucose (8.27 ± 2.90) were within normal ranges. (Table 1).
Changes in knowledge and adherence after the intervention among the respondents
The baseline assessment revealed low baseline knowledge in both groups regarding diabetes and its management. However, after the intervention, there was a significant improvement (P < 0.01) among the intervention group participants. This improvement was notably greater (P < 0.01) compared to the control group across various knowledge components, as indicated by Mean ± SD, such as basic knowledge about diabetes (Baseline: 15.90 ± 10.85, Endline: 26.38 ± 10.41), drug (Baseline: 25.43 ± 27.88, Endline: 48.63 ± 35.07), diet (Baseline: 38.98 ± 26.42, Endline: 53.16 ± 24.18), physical exercise (Baseline: 16.32 ± 15.80, Endline: 34.77 ± 19.05), follow-up visit (Baseline: 8.56 ± 15.33, Endline: 26.38 ± 10.41), foot care (Baseline: 12.44 ± 15.55, Endline: 54.57 ± 45.05), total technical aspects (Baseline: 21.13 ± 14.70, Endline: 43.91 ± 19.13) and total knowledge regarding diabetes (Baseline:17.88 ± 11.11, Endline: 33.02 ± 11.67) (Table 2).
Table 2.
Changes in knowledge and differences between groups after the intervention
|
Knowledge on different components of diabetes
|
Intervention group (n=200)
|
Control group (n=200)
|
Differences between intervention
vs. control group (at end line)
|
|
Baseline
|
End line
|
P
|
Baseline
|
End line
|
P
|
|
Mean±SD
|
Mean±SD
|
Mean±SD
|
Mean±SD
|
P
|
| Total basic knowledge |
15.90 ± 10.85 |
26.38 ± 10.41 |
0.01* |
16.63 ± 11.18 |
17.17 ± 11.52 |
0.06 |
0.01* |
| Drug |
25.43 ± 27.88 |
48.63 ± 35.07 |
0.01* |
28.35 ± 28.75 |
27.75 ± 29.07 |
0.21 |
0.01* |
| Diet |
38.98 ± 26.42 |
53.16 ± 24.18 |
0.01* |
40.34 ± 26.14 |
38.72 ± 26.98 |
0.13 |
0.01* |
| Physical exercise |
16.32 ± 15.80 |
34.77 ± 19.05 |
0.01* |
16.72 ± 15.35 |
17.30 ± 15.75 |
0.19 |
0.01* |
| Follow-up visit |
8.56 ± 15.33 |
22.89 ± 29.57 |
0.01* |
9.69 ± 16.44 |
9.79 ± 16.81 |
0.56 |
0.01* |
| Foot care |
12.44 ± 15.55 |
54.57 ± 45.05 |
0.01* |
13.14 ± 16.03 |
12.18 ± 15.81 |
0.05 |
0.01* |
| Total technical knowledge |
21.13 ± 14.70 |
43.91 ± 19.13 |
0.01* |
22.14 ± 14.18 |
21.62 ± 15.49 |
0.27 |
0.01* |
| Total knowledge on diabetes |
17.88 ± 11.11 |
33.02 ± 11.67 |
0.01* |
18.72 ± 11.51 |
18.86 ± 12.06 |
0.68 |
0.01* |
Data are presented as mean ± standard deviation. A paired t test was used for within-group comparisons and an independent t test was used for group comparisons, with a significance level of *P < 0.05. Adjusted for gender, number of children, family size, family history, used therapy, distance to go to hospital, cost to go to hospital, accompanying person needed, blood pressure (diastolic), and blood glucose (fasting).
Table 3 showed that compared to the control group, the intervention group’s adherence to each component of diabetes management improved significantly (P < 0.01) after intervention. Components like drug (OR = 4.74), diet (OR = 6.06), physical exercise (OR = 5.25), follow-up visit (OR = 4.44), blood glucose test (OR = 3.22), tobacco use (OR = 2.51), foot care (OR = 3.82) and total adherence (OR = 7.98) showed drastic improvement. Although the control group also showed significant improvement in adhesion to drug and total adhesion level, it seems that the total number of respondents is still high in the intervention group compared to the control group (Drug: Intervention endline- 84%, Control endline- 52.6% & total adherence: Intervention endline- 88.7%, Control endline- 49.5%) (Table 3).
Table 3.
Changes in adherence and differences between groups after the intervention
|
Adherence to different components of diabetes management
|
Intervention Group (n=200)
|
Control Group (n=200)
|
After the intervention
|
|
Baseline
|
Endline
|
P
|
Baseline
|
Endline
|
P
|
Odd ratio (95% CI)/
P
|
|
No. (%)
|
No. (%)
|
No. (%)
|
No. (%)
|
| Drug |
83 (42.8) |
163 (84.0) |
0.01* |
87 (44.8) |
102 (52.6) |
0.01* |
4.74 (2.94-7.63)/ 0.01* |
| Diet |
86 (44.3) |
164 (84.5) |
0.01* |
89 (45.9) |
92 (47.4) |
0.54 |
6.06 (3.74-9.80) 0.01* |
| Physical exercise |
50 (25.8) |
139 (71.6) |
0.01* |
58 (29.9) |
63 (32.5) |
0.23 |
5.25 (3.40-8.10) 0.01* |
| Follow-up visit |
49 (25.3) |
127 (65.5) |
0.01* |
54 (27.8) |
58 (29.9) |
0.21 |
4.44 (2.90-6.81) 0.01* |
| Blood glucose test |
71 (36.6) |
138 (71.1) |
0.01* |
78 (40.2) |
84 (43.3) |
0.10 |
3.22 (2.11-4.91) 0.01* |
| Tobacco use |
150 (77.3) |
167 (86.1) |
0.01* |
138(71.1) |
138(71.1) |
1.00 |
2.51 (1.50-4.18)/ 0.01* |
| Foot care |
72 (37.1) |
146 (75.3) |
0.01* |
81 (41.8) |
86 (44.3) |
0.06 |
3.82 (2.48-5.88) 0.01* |
| Total adherence |
88 (45.4) |
172 (88.7) |
0.01* |
86 (44.3) |
96 (49.5) |
0.01* |
7.98 (4.71-13.49) 0.01* |
Data are presented as proportion; n (percentage %). McNemar test was used within-group comparisons and Logistic Regression was used between-group comparisons after one-year intervention with a significance level of *P < 0.05. The adherence level of each parameter was indicated. The control group was the reference category for calculating the odds ratio. Adjusted for gender, number of children, family size, family history, used therapy, distance to go to hospital, cost to go to hospital, accompanying person needed, blood pressure (diastolic), and blood glucose (fasting).
Discussion
This study evaluated the effectiveness of an m-health intervention for diabetes self-management in urban Bangladesh. The intervention involved using the “Diabetes Self-Care” mobile app for six months, emphasizing usability and acceptability. Patients in the intervention group received daily reminders tailored to the seven self-management components of diabetes. Building upon prior studies in Bangladesh, the intervention encompassed a pictorial educational book and a behavior-tracking logbook.4 Utilizing reminder-based tools alongside traditional health education has been recognized as effective in improving knowledge and adherence to diabetes management.18-20,26
In both intervention and control groups, most participants had a family history of DM, received clinical therapy as a treatment and lived within 3 kilometers of healthcare facilities with transport costs below $0.74, indicating an optimistic scenario on the availability of existing healthcare support for diabetic patients. However, many required a need for an accompanying person to go to the hospital may be due to their ill health condition triggered by the comorbidities. Mean blood glucose levels were similar between groups. Baseline survey findings showed no significant correlations between socio-demographic and clinical characteristics, consistent with other studies in Bangladesh.4,16,17
The baseline survey revealed a low mean knowledge level across various diabetes management components in both groups. However, after the intervention, the endline data showed a significant improvement in diabetes self-management knowledge, particularly in the intervention group. Components such as basic knowledge, drug management, diet, exercise, follow-up visits, foot care, and total technical aspects all improved significantly more in the intervention group than the control group. Another study also noted a substantial increase in knowledge parameters among intervention groups, including diet, exercise, follow-up visits, blood glucose monitoring, tobacco cessation, and both basic and technical diabetes management knowledge.22 Traditional interventions like community-based and organization-based counseling have demonstrated efficacy in improving diabetes knowledge worldwide.27-29
The baseline survey revealed poor adherence to the seven diabetes self-management components in nearly half of the cases in both groups. More than half of the participants failed to follow drug and dietary advice, often due to forgetting. Regular exercise was also lacking, primarily due to forgetting. Most participants did not attend scheduled follow-up visits and blood glucose tests, mainly because they forgot. Surprisingly, most claimed to adhere to tobacco cessation advice. Foot care advice was also largely ignored, with forgetting cited as the main reason. The endline survey showed distinct differences between the intervention and control groups in adherence patterns.
After the intervention, the difference in adherence to diabetes self-management between the intervention and control groups was significant. Most of the components of knowledge: drug, diet, physical exercise, follow-up visit, blood glucose test, tobacco use, foot care, and total adherence, substantial significant improvements were observed within the intervention group compared to the control group. The logistic regression analysis revealed a significant improvement in between-group comparisons after a one-year intervention. Significant higher odds regarding greater adherence were found in the components which are drug, diet, physical exercise, and follow-up visit. Consequently, the outcome after intervention showed significantly higher odds of total adherence. In a separate study conducted in Bangladesh, the impact of the intervention was more significant in the m-health education group concerning adherence to four key components (drug, physical exercise, follow-up visit, blood glucose monitoring, and stopping tobacco) and conversely, more crucial in the traditional health education group for diet and foot care practices.22
Our study and others have found significant efficiency and effectiveness in m-Health interventions.18,22,28 Conversely, a prior qualitative study in Dhaka highlighted the role of social and family support in improving adherence to physical exercise. conversely, a prior qualitative study in Dhaka highlighted the role of social and family support in improving adherence to physical exercise.20 However, there is a scarcity of studies assessing the effectiveness of mobile phone applications due to implementation challenges.18,20 An experimental study in urban Bangladesh utilizing voice call services demonstrated significant improvements in drug adherence, physical exercise, timely physician consultations, and tobacco cessation.28,29
The study’s significant and robust outcome strengthens its findings, as the intervention group showed improved knowledge and adherence regarding diabetes. Additionally, the use of a validated questionnaire from a previous study adds to the study’s strength. The intervention tool was found to be user-friendly and well-accepted by participants. A study in Iran also demonstrated that image-based educational interventions improved knowledge and adherence among diabetic patients with lower education levels compared to other groups.29
The study’s limitations include recruiting patients solely from the greater Dhaka city area, limiting the generalizability of the findings to all diabetic patients in Bangladesh. Additionally, a small number of dropouts, some due to unavailability or death, were not significantly different from the study population in terms of basic criteria or variables.
Conclusion
The study showed that m-Health intervention positively impacted patients’ knowledge and adherence, notably improving areas like diet, exercise, tobacco cessation, betel nut cessation, and daily foot care for diabetes self-management. Significant knowledge improvement was observed among the intervention group. The intervention also significantly increased adherence to diabetes self-management components, although minimal changes were seen in healthcare facility visits, likely due to financial constraints. These challenges contributed to uncontrolled blood glucose levels. Implementing a public health insurance system and adding NCD medications to the essential medicine list could alleviate financial barriers. Scaling up m-Health support for diabetic patients is a promising strategy for enhancing adherence and effective condition management. Future studies should explore the long-term sustainability of m-Health interventions in diabetes management and assess their impact on clinical outcomes. For practice, integrating m-Health tools into national healthcare strategies can enhance patient education and adherence, particularly in underserved areas.
Competing Interests
None declared.
Consent for Publication
All respondents permitted publication, provided anonymity was ensured.
Ethical Approval
Ethical approval was taken from the Ethical Review Committee of the Northern University Bangladesh, Dhaka, Bangladesh (NUB/DPH/EC/2022/20-a). Informed written consent was collected from the participants before inclusion in the study. Informed consent was obtained from all participants in the study. The study was performed in line with the principles of the Helsinki Declaration.
Acknowledgements
The study was supported by the Ministry of Science and Technology, Peoples’ Republic of Bangladesh. We acknowledge Savar Swasthoseba Kendro (SSK) and Bangladesh Institute of Health Sciences (BIHS) General Hospital, managed by the Diabetic Association of Bangladesh (BADAS). We are incredibly grateful for the generosity of the patients and their families.
References
- Centers for Disease Control and Prevention (CDC). Increasing prevalence of diagnosed diabetes--United States and Puerto Rico, 1995-2010. MMWR Morb Mortal Wkly Rep.
2012;61(45):918-21.
- Cui M, Wu X, Mao J, Wang X, Nie M. T2DM self-management via smartphone applications: a systematic review and meta-analysis. PLoS One 2016; 11(11):e0166718. doi: 10.1371/journal.pone.0166718 [Crossref] [ Google Scholar]
- IDF Diabetes Atlas. International Diabetes Federation; 2015.
- Banu B, Khan MMH, Ali L, Barnighausen T, Sauerborn R, Souares A. Pattern and predictors of non-adherence to diabetes self-management recommendations among patients in peripheral district of Bangladesh. Trop Med Int Health 2024; 29(3):233-42. doi: 10.1111/tmi.13966 [Crossref] [ Google Scholar]
- Alaslawi H, Berrou I, Al Hamid A, Alhuwail D, Aslanpour Z. Diabetes self-management apps: systematic review of adoption determinants and future research agenda. JMIR Diabetes 2022; 7(3):e28153. doi: 10.2196/28153 [Crossref] [ Google Scholar]
- Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Fischl AH. Diabetes self-management education and support in type 2 diabetes. Diabetes Educ 2017; 43(1):40-53. doi: 10.1177/0145721716689694 [Crossref] [ Google Scholar]
- Das S, Mitra K, Mandal M. Sample size calculation: basic principles. Indian J Anaesth 2016; 60(9):652-6. doi: 10.4103/0019-5049.190621 [Crossref] [ Google Scholar]
- Hex N, Bartlett C, Wright D, Taylor M, Varley D. Estimating the current and future costs of type 1 and type 2 diabetes in the UK, including direct health costs and indirect societal and productivity costs. Diabet Med 2012; 29(7):855-62. doi: 10.1111/j.1464-5491.2012.03698.x [Crossref] [ Google Scholar]
- Bene BA, O’Connor S, Mastellos N, Majeed A, Fadahunsi KP, O’Donoghue J. Impact of mobile health applications on self-management in patients with type 2 diabetes mellitus: protocol of a systematic review. BMJ Open 2019; 9(6):e025714. doi: 10.1136/bmjopen-2018-025714 [Crossref] [ Google Scholar]
- Araszkiewicz A, Zozulinska-Ziolkiewicz D, Pilacinski S, Naskret D, Uruska A, Wierusz-Wysocka B. Baseline diabetic knowledge after 5-day teaching program is an independent predictor of subclinical macroangiopathy in patients with type 1 diabetes (Poznan Prospective Study). Adv Med Sci 2014; 59(2):240-4. doi: 10.1016/j.advms.2013.12.005 [Crossref] [ Google Scholar]
- Diabetic Association of Bangladesh. Projects. 2020. Available from: https://dab-bd.org/page.php?cat_id=6. Accessed June 10, 2020.
- Lau PW, Lau EY, Wong del P, Ransdell L. A systematic review of information and communication technology-based interventions for promoting physical activity behavior change in children and adolescents. J Med Internet Res 2011; 13(3):e48. doi: 10.2196/jmir.1533 [Crossref] [ Google Scholar]
- Boels AM, Vos RC, Dijkhorst-Oei L-T, Rutten GE. Effectiveness of diabetes self-management education and support via a smartphone application in insulin-treated patients with type 2 diabetes: results of a randomized controlled trial (TRIGGER study). BMJ Open Diabetes Res Care 2019; 7(1):e000981. doi: 10.1136/bmjdrc-2019-000981 [Crossref] [ Google Scholar]
- Free C, Phillips G, Felix L, Galli L, Patel V, Edwards P. The effectiveness of M-health technologies for improving health and health services: a systematic review protocol. BMC Res Notes 2010; 3:250. doi: 10.1186/1756-0500-3-250 [Crossref] [ Google Scholar]
- Blythin AM, Elkes J, van Lindholm T, Bhogal A, Wilkinson TM, Saville C. Can digital health apps provide patients with support to promote structured diabetes education and ongoing self-management? A real-world evaluation of myDiabetes usage. Digit Health 2023; 9:20552076221147109. doi: 10.1177/20552076221147109 [Crossref] [ Google Scholar]
- Yasmin F, Nahar N, Banu B, Ali L, Sauerborn R, Souares A. The influence of mobile phone-based health reminders on patient adherence to medications and healthy lifestyle recommendations for effective management of diabetes type 2: a randomized control trial in Dhaka, Bangladesh. BMC Health Serv Res 2020; 20(1):520. doi: 10.1186/s12913-020-05387-z [Crossref] [ Google Scholar]
- Saleh F, Mumu SJ, Ara F, Begum HA, Ali L. Knowledge and self-care practices regarding diabetes among newly diagnosed type 2 diabetics in Bangladesh: a cross-sectional study. BMC Public Health 2012; 12:1112. doi: 10.1186/1471-2458-12-1112 [Crossref] [ Google Scholar]
- El-Gayar O, Timsina P, Nawar N, Eid W. Mobile applications for diabetes self-management: status and potential. J Diabetes Sci Technol 2013; 7(1):247-62. doi: 10.1177/193229681300700130 [Crossref] [ Google Scholar]
- Goyal S, Morita P, Lewis GF, Yu C, Seto E, Cafazzo JA. The systematic design of a behavioural mobile health application for the self-management of type 2 diabetes. Can J Diabetes 2016; 40(1):95-104. doi: 10.1016/j.jcjd.2015.06.007 [Crossref] [ Google Scholar]
- Jeffrey B, Bagala M, Creighton A, Leavey T, Nicholls S, Wood C. Mobile phone applications and their use in the self-management of type 2 diabetes mellitus: a qualitative study among app users and non-app users. Diabetol Metab Syndr 2019; 11:84. doi: 10.1186/s13098-019-0480-4 [Crossref] [ Google Scholar]
- District Statistics Dhaka. Bangladesh Bureau of Statistics, Statistics and Informatics Division, Ministry of Planning, Government of the people’s Republic of Bangladesh; 2013. http://203.112.218.65:8008/WebTestApplication/userfiles/Image/District%20Statistics/Dhaka.pdf. Accessed July 19, 2023.
- Banu B, Ko KC, Khan MM, Ali L, Barnighausen T, Sauerborn R. Effects of traditional versus m-Health educational interventions for diabetic patients: a randomised controlled trial in peripheral district of Bangladesh. Diabet Epidemiol Manag 2023; 9:100106. doi: 10.1016/j.deman.2022.100106 [Crossref] [ Google Scholar]
- Banu B, Chowdhury SH, Akter N, Islam KR, Hossain SM, Amin MR. Preventive behaviors to mitigate COVID-19: urban-rural disparities of densely populated country like Bangladesh. J Environ Sci Public Health 2021; 5(4):433-50. doi: 10.26502/jesph.96120142 [Crossref] [ Google Scholar]
- American College of Cardiology. Blood Pressure Categories from 2017 High Blood Pressure Guidelines. 2019. https://www.acc.org/latest-in-cardiology/ten-points-to-remember/2017/11/09/11/41/2017-guideline-for-high-blood-pressure-in-adults. Accessed March 1, 2021.
- Diabetes.co.uk. Normal and Diabetic Blood Sugar Level Ranges. 2018. https://www.diabetes.co.uk/diabetes_care/blood-sugar-level-ranges.html. Accessed March 1, 2021.
- Kebede MM, Pischke CR. Popular diabetes apps and the impact of diabetes app use on self-care behaviour: a survey among the digital community of persons with diabetes on social media. Front Endocrinol (Lausanne) 2019; 10:135. doi: 10.3389/fendo.2019.00135 [Crossref] [ Google Scholar]
- World Health Organization (WHO). Countries: Bangladesh. 2017. http://www.who.int/countries/bgd/en/. Accessed June 23, 2023.
- Agarwal P, Mukerji G, Desveaux L, Ivers NM, Bhattacharyya O, Hensel JM. Mobile app for improved self-management of type 2 diabetes: multicenter pragmatic randomized controlled trial. JMIR Mhealth Uhealth 2019; 7(1):e10321. doi: 10.2196/10321 [Crossref] [ Google Scholar]
- Rangraz Jeddi F, Nabovati E, Hamidi R, Sharif R. Mobile phone usage in patients with type II diabetes and their intention to use it for self-management: a cross-sectional study in Iran. BMC Med Inform Decis Mak 2020; 20(1):24. doi: 10.1186/s12911-020-1038-y [Crossref] [ Google Scholar]